Meet our new Postpartum Doula and Newborn Care Specialist (NCS), Sarah!

We hope you enjoy getting to know Sarah in our Q&A blog! Sarah serves families in West Michigan as a certified Newborn Care Specialist. She offers day and overnight newborn support. 1) What did you do before you became a newborn care specialist? I have worked in the field of Early Childhood for 20 […]
Meet Mya, Our Newest Postpartum Doula!

Meet Mya, Our Newest Postpartum Doula! As you know, when we bring a new person onto the Gold Coast team, we love to find out more about them and share that with you! Let’s find out more about Mya. 1) What did you do before you became a postpartum doula? Before becoming a doula, I […]
2022 Reflections

2022 Reflections: Whew! Our word of the year for 2022 was changed. Gold Coast announced an expansion for day and overnight postpartum support to Northern and Southwest Michigan in April. Alyssa Veneklase transitioned from co-owner to subcontractor at Gold Coast in August. She still leads the Becoming A Mother course with Kristin and teaches at […]
Why You Should Take a Breastfeeding Class: Podcast Episode #166

Kristin chats with Kelly Emery of Baby Beloved about why moms should take a breastfeeding class during pregnancy. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about […]
Meet our new Postpartum Doula, Jene’e!

1) What did you do before you became a doula/consultant? For many years, I primarily have been a “domestic engineer”, a stay-at-home mom. Although in some of those years, my family has owned a few restaurants, and I helped there when I was needed. 2) What inspired you to become a doula/consultant? Becoming a mama […]
Top 5 Tips for Encouraging Baby to Sleep Through the Night

Kay Vorce, CED-PIC Gold Coast Sleep Consultant If there is one question I get all the time, it’s this one: How can I encourage my baby to sleep through the night while still responding to their needs? First, let’s define what that means. If your baby is sleeping 6-8 hour stretches, that’s considered sleeping […]
2022 Diaper Drive Numbers Are In!

The final numbers are in for the Gold Coast Doulas LLC diaper drive for Nestlings | Diaper Bank of West Michigan. We collected 11,133 disposable diapers and 97 packs of wipes. These diapers are packed in groups of ten to impact families in need. We are thankful to all of our clients and community members who donated from September 1st to October 2rd during […]
Acupuncture during Pregnancy and Postpartum: Podcast Episode #103

Dr. Carrie Dennie, ND speaks with Alyssa about the benefits of acupuncture during pregnancy and postpartum. You can listen to this complete podcast episode on iTunes or SoundCloud. Alyssa: Welcome to the Ask the Doulas Podcast. You are listening to Alyssa Veneklase. I am the co-owner of Gold Coast Doulas, and today, I am […]
Fertility and Acupuncture: Podcast Episode #101

Today Kristin talks to Vikki Nestico, R.Ac of Grand Wellness Acupuncture. We learn a lot about fertility and how acupuncture supports the nervous system, reduces stress, and increases blood flow to the reproductive organs. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Hi, Vikki! Vikki: Hi, how are you? […]
Signs of Early Pregnancy

This blog is written by Jessica Kupres, BSN, RN, CLC, CBE a Postpartum Doula with Gold Coast. As you lie in bed thinking about your day and putting your brain to rest, you might think about the great presentation you gave today. Did you put the clothes in the dryer? When was your last period?…. […]
Hyperemesis Gravidarum

This post was written by Lauren Utter, a ProDoula trained Birth and Postpartum Doula with Gold Coast Doulas. Finding out you are pregnant can bring an array of emotions – planned pregnancy or not. Maybe you’re excited because you have been waiting for this day. Maybe you are surprised because a baby wasn’t on your […]
Planning a Nursery During the COVID-19 Pandemic

Today’s guest blog is written by Isabella Caprario, Content Marketing Specialist at Porch. During the COVID-19 pandemic, we all feel uncertainty. We don’t know what will happen or what steps to take next. We only know that the best way to end this madness is to sit at home and take all the necessary precautions […]
COVID-19 Reduce Your Risk!

Ask The Doulas Podcast · Corona Virus Update on Doulas Reduce Your Risk by Megan Mouser, NP. March 31, 2020 STATISTICS COVID-19 With statistics regarding the novel coronavirus changing daily (and even hourly), the most up-to-date information can come from Michigan Department of Health and Human Services as well as the Centers for Disease […]
A Journey Unlike Any Other

To all of the couples who have had retrievals, transfers, and IVF schedules postponed or affected by the Corona virus outbreak my heart breaks for you. IVF is no small or easy journey; it takes a toll on your mental, emotional, and physical state. It’s beautiful and terrifying all at the same time. It’s expensive […]
Staying Fit and Healthy During Your Pregnancy

My name is Kaysie, and I am currently 20 weeks pregnant. This is my 4th pregnancy and the first one where I have maintained a very healthy and fit lifestyle. I am a mom of three – 16, 13, and 7. After my last child was born I was the heaviest I had ever been […]
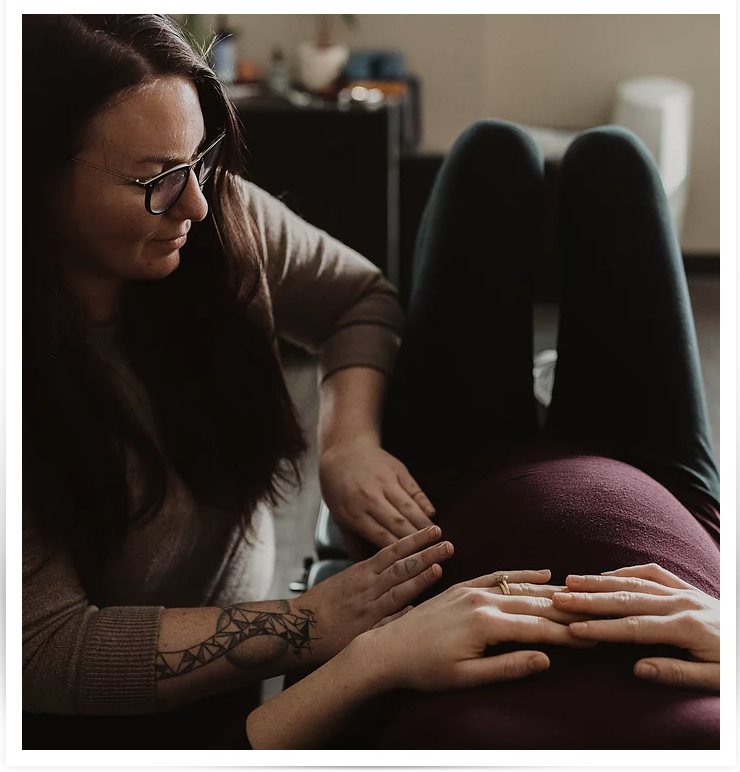
Physical Therapy During Pregnancy
Maternity clothes✓ Registry✓ Hospital tour✓ Doula✓ Photographer✓ What could you possibly be forgetting? What about getting YOURSELF prepared? Likely from the moment you found out you were pregnant you have been focused on the tiny human growing inside of you. While prenatal vitamins, nursery preparations, and choosing the perfect name are all very important parts […]
Symphysis Pubis Dysfunction with Rise Wellness Chiropractic: Podcast Episode #90
Dr. Annie and Dr. Rachel talk to Alyssa about Symphysis Pubis Dysfunction (SPD), how to prevent it, how to treat it, and things every pregnant and postpartum woman should be doing! You can listen to this complete podcast episode on iTunes or SoundCloud. Hello. Welcome to another episode of Ask the Doulas. I am Alyssa, […]
Baby-Friendly Hospital Initiative: Podcast Episode #89

Today we speak with Katie and Becky from Spectrum Health in Grand Rapids about what it means to be a designated Baby-Friendly hospital. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the Doulas with Gold Coast Doulas. I’m Kristin, co-owner, and I’ve got Alyssa here. And we’ve […]
Saving for Baby: Podcast Episode #88

Kristin talks to Paige, The Millennial Guru, again today about how to financially prepare for growing your family! You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the Doulas with Gold Coast Doulas. I’m Kristin, co-owner of Gold Coast, and I’ve got Paige Cornetet, the Millennial Guru, here […]
The Millennial Guru: Podcast Episode #87

Paige, The Millennial Guru, shares some savvy saving tips to help you think about priorities, wants, and needs and how to budget for them. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the Doulas with Gold Coast Doulas. I’m Kristin, co-owner, and I’m here today with Paige […]
Preparing Your Body For Pregnancy: Podcast Episode #84

Dr. Nave now works with queens through her virtual practice Hormonal Balance. We talk this time about how a woman can prepare her body for pregnancy. You can listen to this complete podcast episode on iTunes or SoundCloud. Alyssa: Hello! Welcome to another episode of Ask the Doulas Podcast. You have Kristin and Alyssa here […]
Maddie’s Birth Story: Podcast Episode #83

Our listeners love hearing a positive birth story. Today Maddie, a previous HypnoBirthing and Birth client, tells us all about her labor and delivery as well as her experience in the hospital right after having her baby. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the Doulas […]
How Sleep Deprivation Impacts New Parents

Becoming a parent is one of the most exciting and scary milestones of a person’s life. It’s likely your emotions will run the gamut from excited anticipation and joy, to fear of the unknown and uncertainty about what’s ahead and how you’re coping with parenthood. Managing night time feeds, tending to your baby throughout the […]
Understanding Your Cycle: Podcast Episode #82

Dr. Nave now works with queens through her virtual practice Hormonal Balance. She talks with us today about a woman’s monthly cycle. What’s “normal”? What if you don’t get a period at all? Is PMS a real thing? You can listen to this complete podcast episode on iTunes or SoundCloud. Alyssa: Hello, welcome to Ask […]


