Amanda Tice and The New Mom Code – podcast episode #139

Amanda Tice, model and author, talks about becoming a new mom. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you get your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics related to pregnancy, birth, postpartum, and […]
Juliet’s Personal Preeclampsia Story: Podcast Episode #138

Juliet Meyer shares her personal preeclampsia story with Kristin that led to her work with the Preeclampsia Foundation. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you get your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about […]
Elizabeth King, Fertility Coach: Podcast Episode #137

Elizabeth King, Fertility Coach, shares helpful tips and resources for those who are struggling with conception and loss. You can listen to this complete podcast on iTunes, SoundCloud, or wherever you get your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics […]
Amber’s VBAC Story: Podcast Episode #136

Kristin chats with Gold Coast client Amber Shaw about her VBAC birth story and the preparation she had for her birth. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over […]
Ask Dr. Mom: Podcast Episode #135
Kristin talks with Dr. Elham Raker about telemedicine in times of COVID and offers parenting tips for mothers . Dr. Elham is the official “Ask Dr. Mom” who has leveraged her experience as a pediatrician to help parents navigate the “shoulds” of motherhood. Welcome. You’re listening to Ask the Doulas, a podcast where we talk […]
Train for birth the way you would for an Ironman: Podcast Episode #134

Dave Howlett, founder of Real Human Being, talks to us about how elite athletes prepare mentally and physically and so should parents before birth. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts […]
Talking About Tricky Topics With Your Caregivers: Podcast Episode #133

Today we discuss the importance of having difficult conversations with your nanny or caregiver. Joining us is Carol Kramer Arsenault of Boston Baby Nurse & Nanny. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you listen to podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk […]
Cord Blood Banking: Podcast Episode #132

Today, we sit down with Kathryn Cross, CEO & Founder of Anja Health to discuss the importance and practical uses of umbilical cord blood. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you listen to podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts […]
Pelvic Floor: Managing Pain with Intercourse – Podcast Episode #131

Joining us today is Amanda Seymour and Katie Thomas from Hulst Jepsen Physical Therapy. We discuss the issue of painful intercourse, its causes and the importance of speaking up among those who are impacted. You can listen to this complete podcast episode on iTunes, Spotify, or SoundCloud. Welcome. You’re listening to Ask the Doulas, a […]
Managing a High-Risk Pregnancy: Podcast Episode #130

Kristin and Alyssa talk with Nathalie Walton, CEO of the Expectful App about managing a high risk pregnancy. Go to www.expectful.com/ask-the-doulas promocode ASKDOULAS to get your first month of Expectful for just $1. You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast where […]
Depression, Depletion, and Mourning Our Previous Life: Podcast Episode #129

Alyssa talks with Maranda Bower, Postpartum Bliss Coach, about the difference between depression, depletion, and mourning our previous life. How do our bodies change during pregnancy and how can we best support healing? You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast where […]
Birth Coach Method: Podcast Episode #128
Kristin talks with Neri Life Choma, Author and Founder of Birth Coach Method. They discuss the difference between a Childbirth Educator, Birth Doula, and a Birth Coach. They also talk about transforming birthing person’s expectations from the “perfect natural birth” to a “positive birth experience.” You can listen to this complete podcast episode on iTunes […]
Postpartum Physical Therapy: Podcast Episode #127

Alyssa talks with Amanda and Katie, Women’s Health Physical Therapists at Hulst Jepsen Physical Therapy, about postpartum physical therapy and what pelvic floor physical therapy looks like after having a baby. We talk about incontinence, diastasis recti, symphysis pubic dysfunction, constipation, and so much more! You can listen to this complete podcast episode on iTunes […]
Becoming a Mother: Sarah’s Story – Podcast Episode #126

Kristin talks with Sarah Baker, a current client and student in our BECOMING a Mother course, about her concerns with her second pregnancy/delivery and why she chose to hire a birth doula as well as invest the time in a 6-week online course. Welcome. You’re listening to Ask the Doulas, a podcast where we talk […]
The BECOMING Course: Amber’s Story – Podcast Episode #125

Kristin & Alyssa talk with Amber Shaw, a recent student in The BECOMING a Mother online series of classes, about some fears she had with her second pregnancy and why she took this course. You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast […]
The Lymph System and MLD Therapy: Podcast Episode #124

Kristin talks with Megan Michelotti CD (DONA) about the lymph system and manual lymphatic drainage (MLD) and how it can be helpful prenatally as well as postpartum. You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all […]
Natural Hospital Birth: Podcast Episode #123

Kristin Revere, co-owner of Gold Coast Doulas talks with Cynthia Gabriel, author of Natural Hospital Birth, about her experience as a doula and health care provider for women, supporting natural hospital births. You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast where we […]
What is Art Therapy? Podcast Episode #122
Alyssa talks with Janna VanderBand, an art therapist in West Michigan. We learn what art therapy is and how mothers, in any stage of their journey from fertility and conception to pregnancy and postpartum, can use art therapy to heal. You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening […]
Welcome to Fatherhood: Podcast Episode #121

Kristin talks with David Arrell, author of Welcome to Fatherhood. He talks about why he wrote the book then gets into some great tips for Dads and how to best support Mom! This one is a must listen! You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask […]
Urinary Incontinence: Podcast Episode #120

Amber and Katie from Hulst Jepsen Physical Therapy talk with Alyssa again about women’s health pelvic floor rehab with a focus on urinary incontinence. You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country […]
Valerie Lynn – The Mommy Plan: Podcast Episode #119

What is eco postnatal care? Valerie Lynn, author of The Mommy Plan, tells us how to nourish and heal a postpartum body. You can listen to this complete podcast on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics related […]
The Postnatal Cookbook: Podcast Episode #118
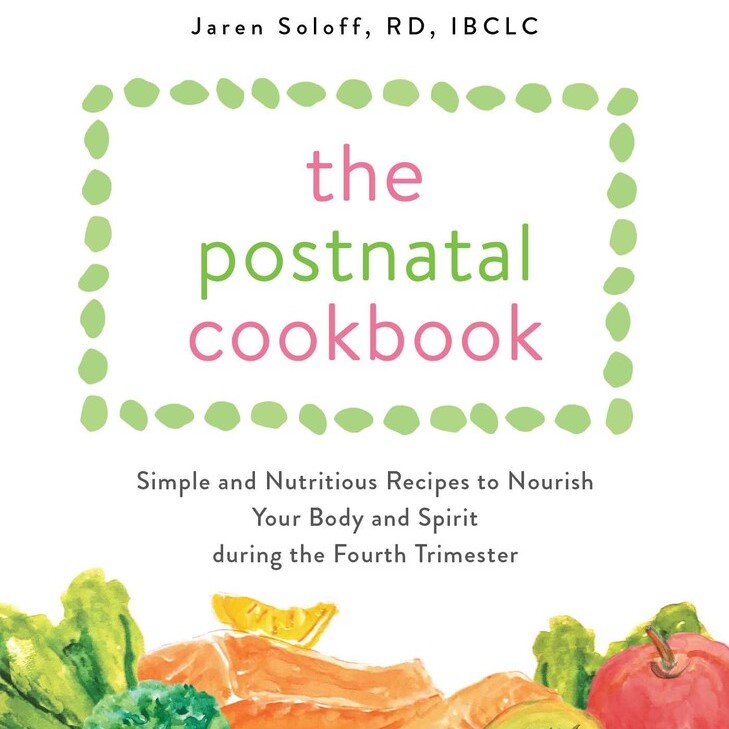
Jaren Soloff RD, IBCLC talks to Kristin about her new book The Postnatal Cookbook and the importance of nutrition during pregnancy and especially postpartum. You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask The Doulas, a podcast where we talk to experts from all over the country […]
Don’t be scared of pelvic floor physical therapy! Podcast episode #117

Amanda and Katie, women’s health physical therapists at Hulst Jepsen Physical Therapy, give us an intro into pelvic floor PT. What is it, what does an internal vs external pelvic floor exam involve, and what kinds of symptoms can pelvic floor PT treat? You can listen to this complete podcast episode on iTunes or SoundCloud. […]
Keeping Yourself Healthy During Pregnancy: Podcast Episode #116

Kristin talks with Dr. Annie of Rise Wellness Chiropractic about how to keep yourself and your family healthy during pregnancy and a pandemic! You can listen to this complete podcast episode on iTunes or SoundCloud. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about […]


