Postpartum Support with Carrie Kolehouse of MomsBloom: Podcast Episode #167

Carrie Kolehouse, Executive Director of MomsBloom chats with Kristin about why MomsBloom is focused on supporting mothers in West Michigan and beyond. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all […]
Meet Mya, Our Newest Postpartum Doula!

Meet Mya, Our Newest Postpartum Doula! As you know, when we bring a new person onto the Gold Coast team, we love to find out more about them and share that with you! Let’s find out more about Mya. 1) What did you do before you became a postpartum doula? Before becoming a doula, I […]
Connection and Compassion Are Key

I’ve said it a lot; there is no one-size-fits-all solution to sleep, but this applies to parenting in general as well. Many parents will read about certain techniques, and even follow specific scripts with older children, but if they don’t work, parents feel like they have failed or there is something wrong with their kid. […]
2022 Reflections

2022 Reflections: Whew! Our word of the year for 2022 was changed. Gold Coast announced an expansion for day and overnight postpartum support to Northern and Southwest Michigan in April. Alyssa Veneklase transitioned from co-owner to subcontractor at Gold Coast in August. She still leads the Becoming A Mother course with Kristin and teaches at […]
Why You Should Take a Breastfeeding Class: Podcast Episode #166

Kristin chats with Kelly Emery of Baby Beloved about why moms should take a breastfeeding class during pregnancy. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about […]
How to Build Foundations to Stay Active Postpartum: Podcast Episode #165

Kristin chats with Dr. Karlie Causey, co-founder of a postpartum activewear brand called Jen & Keri, a sports chiropractor and certified strength and condition coach who is passionate about providing practical tools to moms and moms-to-be, helping them restore their bodies and continue exercising after their babies are born. You can listen to this complete […]
Navigating Healthcare Systems During Pregnancy: Podcast Episode #164

We talk with Estelle Giraud, CEO and co-founder of Trellis Health, about navigating healthcare systems during pregnancy. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics […]
Sign Language for Newborns, Infants, and Toddlers: Podcast Episode #163

We talk with Cara Tyrrell about using sign language with newborns, infants, and toddlers. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Be sure to listen to find out how to get a free download on the benefits of ASL for your little ones! Welcome. You’re […]
Body Image And Nutrition During Pregnancy: Podcast Episode #162

Kristin and English Goldsborough chat about body image during pregnancy and the importance of nutrition. English owns The Nourishing Tree and is a functional nutritional therapy practitioner and a certified lactation counselor. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the […]
NICU and Preemie Mom Support with Jodi Klaristenfeld: Podcast Episode #161

We chat with Jodi Klaristenfeld, founder of FLRRiSH, about navigating the NICU and supporting moms of preemies. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics […]
Fitness Tips for Prenatal and Postnatal: Podcast Episode #160
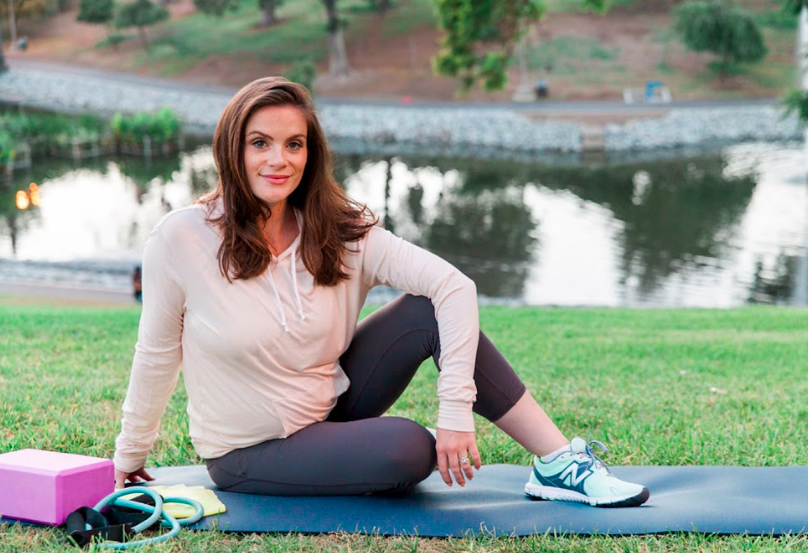
Kristin interviews Sarah Ann Kelly. Sarah Ann is the owner and founder of MomTrainer. Sarah Ann shares prenatal and postnatal fitness tips and suggests ways to create intentional time for working out. Sarah Ann is also giving 50% off with the discount code GoldCoastDoulas! Welcome. You’re listening to Ask the Doulas, a podcast where we […]
Postpartum Anxiety and OCD: Podcast Episode #159

Kristin chats with Jasmine Emerick about her personal struggles with postpartum anxiety and OCD and her work as a therapist. Jasmine is the author of The Postpartum Therapist. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics related to pregnancy, birth, postpartum, and […]
Meet our new Postpartum Doula, Jene’e!

1) What did you do before you became a doula/consultant? For many years, I primarily have been a “domestic engineer”, a stay-at-home mom. Although in some of those years, my family has owned a few restaurants, and I helped there when I was needed. 2) What inspired you to become a doula/consultant? Becoming a mama […]
Potty Training with Christine Brown: Episode #158

Kristin and Christine Brown, owner of Bella Luna Family, discuss top potty training tips and infant sleep. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics related to pregnancy, birth, postpartum, and early parenting. Let’s chat! Kristin: Hello, hello. This is Kristin with […]
Simplifying Motherhood: Podcast Episode #157

Krista Lockwood, founder of Motherhood Simplified, shares her top decluttering tips for new moms to prep for the arrival of a new baby. You can listen to this complete podcast episode on iTunes, SoundCloud, or anywhere you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from […]
Functional Maternity: Podcast Episode #156

Sarah Thompson, author of Functional Maternity explains what maternal functional medicine is and the role nutrition plays in pregnancy and birth outcomes. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all […]
Pilates for Prenatal and Postpartum: Podcast Episode #155

We talk about Pilates with Emma Jory of ePilates Online shares tips on how to take care of your body in all four trimesters. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts […]
Transitioning Back To Work: Podcast Episode #154

Sasha Morozov of Sasha x Home shares top tips for transitioning back to work after having a baby. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about […]
The Ins and Outs of My Vagina with Karin Freeland: Podcast Episode #153
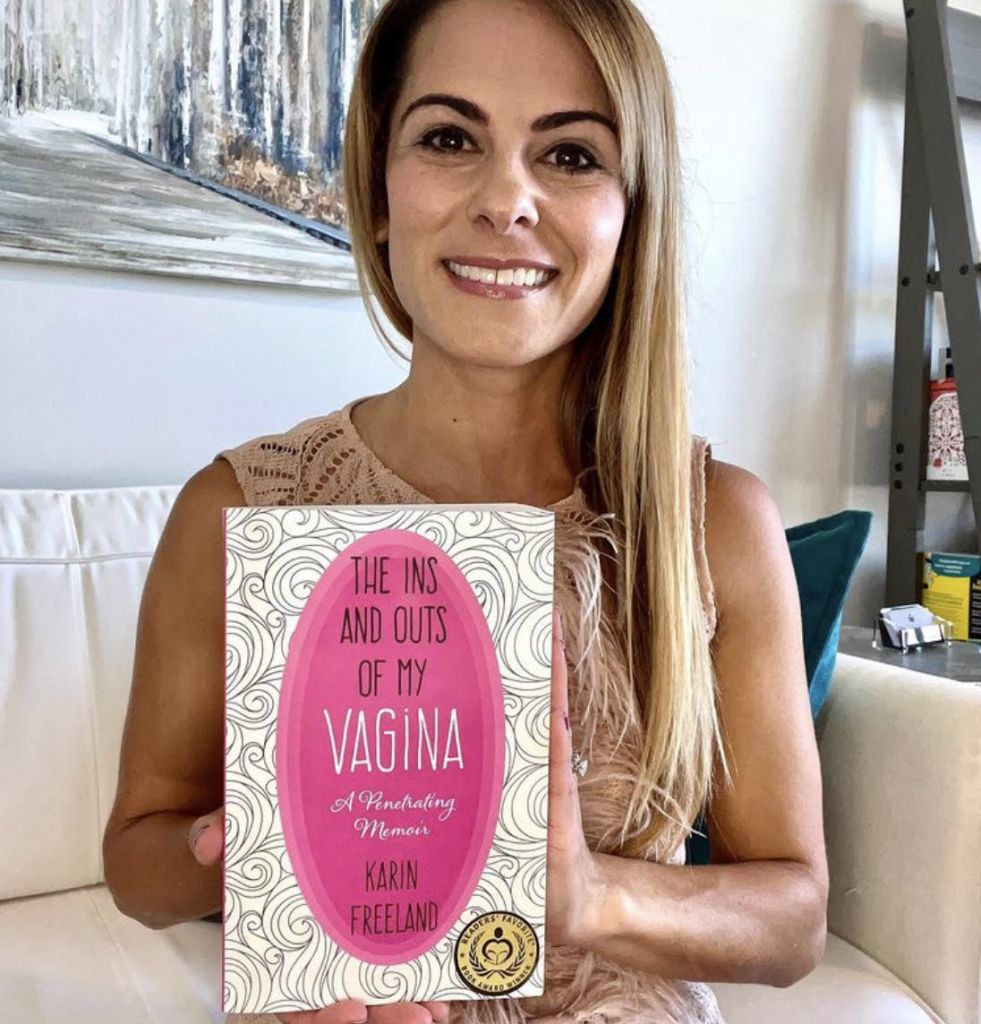
Karin Freeland chats about her book, “The Ins and Outs of My Vagina: A Penetrating Memoir” with Kristin. They discuss everything from body image to postpartum depression. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we […]
Pregnancy Loss

Remember the story of Pandora’s Box? In Greek mythology, the story goes something like this: Pandora, told she could not open the lid of a box given to her or her husband from Zeus, finally lets curiosity get the best of her and opens the box. Immediately, out comes all the troubles that humanity would […]
Autumn To-Do: 5 Ways to Optimize Finances

Summertime is drawing to a quick close! As we ease back into the school year, gear up for holiday seasons, and bid adieu to 2022, the following are some tips that our wealth management clients have found valuable to incorporate. It may feel like spare moments are dwindling in the final weeks of summer, but […]
How to raise perfectly imperfect kids with Lisa Sugarman: Podcast Episode #152

Lisa Sugarman, author of How To Raise Perfectly Imperfect Kids, discusses positive parenting and balance with Kristin. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics […]
Intentional Motherhood with Monique Russell: Podcast Episode #152
Kristin and Monique, author of Intentional Motherhood: Who Said It Would Be Easy?, discuss her book and share tips to connect with your children and communicate your needs with others to better enjoy this time of transition. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. […]
Ayurvedic Postpartum Healing with Ameya Duprey: Podcast Episode #151

Kristin and Ameya Duprey discuss the root causes of postpartum imbalances and how to heal them. Ameya is an Ayurvedic practitioner, postpartum doula and author. You can listen to this complete podcast episode on SoundCloud, iTunes, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to […]
