Acts of Kindness Embryo Donation: Podcast Episode #263

Kristin Revere and Jayme Bess discuss the options for embryo donation for families and the benefits for donors in this informative episode. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Jayme Bess today about embryo donation. Jayme is the founder and CEO of Acts of Kindness […]
All About Vaginal Birth After Cesarean: Podcast Episode #262

Kristin Revere and Meagan Heaton discuss VBAC preparation for families and tips for doulas supporting VBACs in this informative episode of Ask the Doulas. Meagan is the CEO of VBAC Link. Hello, hello. This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with my new friend Meagan Heaton. Our topic […]
Cholestasis and Listening to Your Intuition: Podcast Episode #261

Jenn Johnson shares her personal pregnancy stories and discusses how even as a nurse she had to advocate for herself during pregnancy. Jenn also shared info on her book, A Nurse’s Happy Place. Hello, hello! This is Kristin with Ask the Doulas, and I am thrilled to chat with Jenn Johnson today. Jenn is the owner […]
Feeling Confident in Your Postpartum Body, with Kaylie of Tender Seasons: Podcast Episode #260

Kristin Revere and Kayli Joann discuss Kayli’s entrepreneurial journey, which started out of her frustration with finding postpartum bras and nightgowns that made her feel beautiful. She decided to create her own line of clothing, Tender Seasons. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Kayli […]
Pumping Tips with Jacque Ordner of Motif Medical: Podcast Episode #259

Kristin Revere and Jacque Ordner discuss finding ways to make pumping more effective, comfortable, and sustainable in the latest episode of Ask the Doulas. Jacque is an IBCLC, BSN, RN, RLC, and Motif Medical Advisor. Hello, hello! This is Kristin Revere with Ask the Doulas. I am thrilled to chat with Jacque Ordner today. Jacque […]
Feeding Tips for Parents with Dr. Ari Brown: Podcast Episode #258

Kristin Revere and Dr. Ari Brown focus on the benefits of goat milk formula on the latest episode of Ask the Doulas. Dr. Brown is the chief medical advisor at Kabrita. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Dr. Ari Brown. Dr. Brown is a […]
The Benefits of Doula Care with Laura Navaquin: Podcast Episode #257

Laura Navaquin shares her experience utilizing doula support in the latest episode of Ask the Doulas. She also talks about her work with Nava Consulting and Inspire Her Foundation. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am so excited to chat with Laura Navaquin today. Laura is the founder of […]
Postpartum Wellness with Dr. Emilie Wilson: Podcast Episode #256

Kristin Revere and Dr. Emilie Wilson discuss the importance of preparing for postpartum during pregnancy on the latest episode of Ask the Doulas. Dr. Wilson also shares self-care tips from her new book, “POST: The Essential Guide to Creating Your Postpartum Self-Care Plan in Pregnancy.” Hello, hello! This is Kristin Revere with Ask the Doulas, […]
Early Language Development Strategies with Jeaneen Tang: Podcast Episode #255
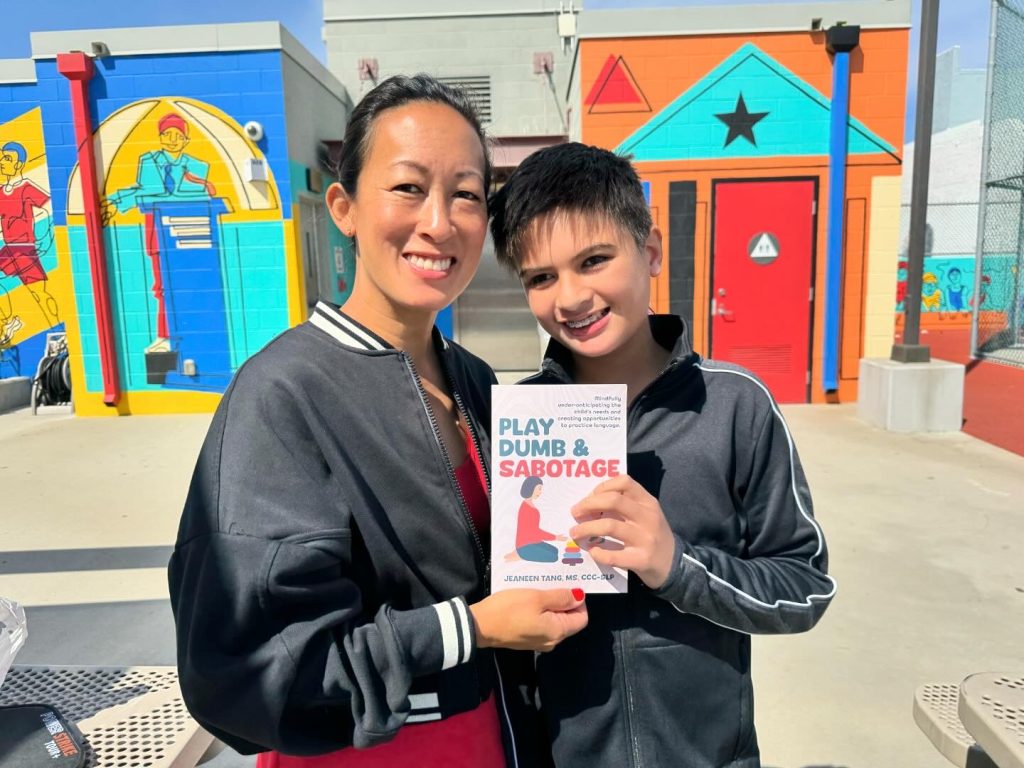
Kristin Revere and Jeaneen Tang discuss how parent and caregiver education and training on early language development skills and strategies is so important. Jeaneen also shares tips from her new book, Play Dumb and Sabotage. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am excited to chat with Jeaneen Tang today. Jeaneen […]
Preparing for Parental Leave: Podcast Episode #254

Kristin Revere and Jackie Cook discuss her work with clients and employers on maternity leave preparation and her Expecting Success program on the latest episode of Ask the Doulas. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with my friend Jackie Cook today. I met Jackie back […]
Preparing for Your Hospital Birth: Podcast Episode #253

Anna Rodney shares hospital birth prep tips with Kristin Revere in the latest episode of Ask the Doulas. Anna is the founder of Birth and Baby University. Gold Coast Doulas is an affiliate for the online Birth and Baby University class, Preparing for Your Hospital Birth. Hello, hello! This is Kristin with Ask the Doulas, […]
Child loss with Christi Kmecik of Written Hugs Designs: Podcast Episode #252

Christi Kmecik shares her journey with loss and how she was drawn to create a beautiful line of grief cards. She also gives tips on how to support someone who is grieving. Hello, hello! This is Kristin with Ask the Doulas, and I am excited to chat with my friend Christi Kmecik. Christi is the […]
Breast Milk Sharing with Kelly Cox of Share the Drop: Podcast Episode #251

Kristin Revere and Kelly Cox discuss milk sharing and her new platform called Share the Drop on the latest episode of Ask the Doulas. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Kelly Cox today. Kelly is a registered prenatal yoga teacher, a birth doula, […]
Health Tips for New and Seasoned Moms with Dr. Lora Grasso: Podcast Episode #250

Kristin Revere and Dr. Lora Grasso discusses small changes that can help you maintain your health after having a baby in the latest episode of Ask the Doulas. Dr. Grasso is the founder of APEX Coaching. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am so excited to chat with my […]
Our Journey to Creating an Audiobook for Supported: Podcast Episode #249

In the latest episode of Ask the Doulas, Kristin Revere discusses the launch of the Audiobook for Supported: Your Guide to Birth and Baby. Alyssa Veneklase and Kristin Revere recorded the audiobook at a local recording studio called Centennial Sound and had a lot of fun with the process. You can now order Supported: Your Guide […]
Spirituality and Doula work with Sabia Wade: Podcast Episode #248

Kristin Revere and Sabia Wade discuss her book “Birthing Liberation” and discuss spirituality and doula work. Sabia is the CEO of Birthing Advocacy Trainings and a speaker, mentor, and author. Hello, hello! This is Kristin with Ask the Doulas, and I am excited to bring back my friend Sabia Wade to Ask the Doulas. […]
Preparing for the Postpartum Phase with Mariela De Santiago: Podcast Episode #247

Kristin Revere and Mariela De Santiago discuss how preparation during pregnancy can impact your postnatal recovery phase. Mariela hosts the New Mom Podcast and is the founder of the Carlsbad Mom Crew. Hello, hello! This is Kristin with Ask the Doulas, and I am thrilled to chat with Mariela De Santiago today. Mariela is the […]
Healing Childhood Trauma in Early Parenting: Podcast Episode #246

Emily Cleghorn shares her personal story of overcoming trauma and discusses the importance of support during motherhood on the latest episode of Ask the Doulas. She also discusses navigating triggers and tantrums as you heal your childhood trauma in the midst of early parenting. Emily is the founder of Mindful Soul Wellness. Hello! This is […]
Surrogacy Simplified: Podcast Episode #244

Kristin Revere and Jessie Jaskulsky discuss the types of surrogacy and options for families in this informative Ask the Doulas episode. Jessie also gives her top tips for families who are considering surrogacy. Jessi owns Surrogacy Simplified. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Jessie […]
Reimagining Care for New Moms with Alexandra Francis: Podcast Episode #243

Kristin Revere and Alexandra Francis discuss postpartum recovery traditions worldwide and the need for holistic postpartum support models like Mama Haven. Alexandra also owns Our Hummingbird. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to bring you Alexandra Francis. Alexandra is the owner and founder of Our Hummingbird, and […]
Postnatal nutrition with Genevieve Mena of Mamieli: Podcast Episode #242

The importance of postnatal nutrition with Genevieve Mena, Co-Founder and CEO of Mamieli. Kristin Revere and Genevieve Mena discuss everything from traveling with kids to nourishing ourselves during the postpartum recovery phase on the latest episode of Ask the Doulas podcast. Be sure to tune in until the end for the special discount code for […]
Changes in Michigan’s Surrogacy Laws: Podcast Episode #241

Kristin Revere and Jessie Jaskulsky of Surrogacy Simplified discuss the changes in Michigan’s Surrogacy laws on the latest episode of Ask the Doulas. Jessie also provides helpful tips to our listeners considering surrogacy as an option to grow their families. Hello! This is Kristin Revere with Ask the Doulas, and I am excited to chat […]
Craniosacral Therapy for Infants with Meaghan Beames: Podcast Episode #240

Kristin Revere talks with Meaghan Beames of MyBaby Craniosacral Podcast and Beames CST Training Centre. They discuss how craniosacral therapy can help babies cope with colic, latching issues, and growing pains that can make life with a newborn harder than it needs to be. Hello, hello! This is Kristin Revere with Ask […]
How to Build Your Birth and Postpartum Support Team

Kristin Revere was a guest on the Plus Mommy podcast to talk about setting yourself up for success by creating a strong support team for birth and postpartum. Listen to the podcast here. A strong support team can significantly impact your overall experience and well-being, from physical and emotional support to guidance through the complexities […]
