Podcast Episode #63: What is a Speech Therapist?

We’ve all heard of a speech therapist but what do they actually do? In this episode, Courtney Joesel of Building Blocks Therapy Services tells us how speech and language services can benefit a child and why, if you notice signs of speech delay, it’s important to have your child seen earlier rather than later. She […]
Podcast Episode #60: A Naturopath’s Perspective on Pregnancy and Depression

Doctor Janna Hibler, ND talks to Alyssa and Kristin about how a naturopathic doctor treats pregnant and postpartum women, body and mind. You can listen to this complete podcast episode on iTunes and SoundCloud. Alyssa: Hello, welcome to Ask the Doulas podcast. I am Alyssa Veneklase, co-owner of Gold Coast Doulas, and I am here […]
Doula Support for Adoptive Families

Most parents probably don’t think about hiring a doula if they aren’t pregnant. They think of a birth doula only supporting a laboring mother, but that couldn’t be farther from reality. Birth doulas can support any parent. Postpartum doulas can support adoptive families by helping them to prepare for baby’s arrival and in-home after baby […]
The Most Wonderful Time of The Year…or is it?

On of our birth doulas, Angel, reflects on this holiday season as a mother with a newborn. I think alot of us can relate… So you recently popped out a baby. Maybe your first, maybe your last. Either way, you are probably feeling a bit like you’re treading water. I know. I feel it too. […]
Nursing & The Entrepreneur

Today’s guest blog is from our dear friend, Kristina Bird. She is a partner with The People Picture Company, a photography studio located in the heart of downtown Grand Rapids committed to producing magazine quality photography for all of life’s milestones. Sitting in my car, the beating hum of my pump out of sync with […]
Mothership Certified Health Service Providers
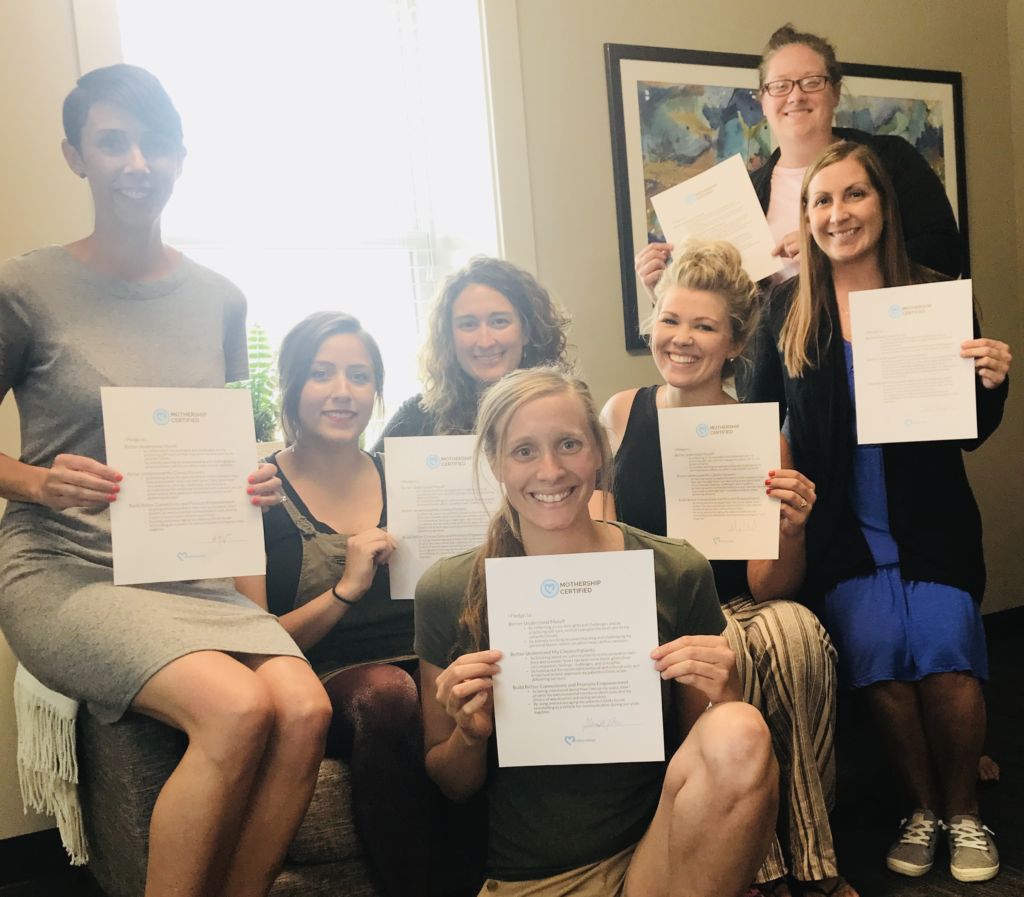
Many of our doulas are Mothership Certified Health Service Providers. Sounds cool, but what does that mean? Here’s a simplified breakdown of what we learned in our training and why it’s so important. The training involved learning the difference between empathy and sympathy. We understand that empathy never starts with, “At least…”. Here’s a great […]
My role as a postpartum doula.

Our very own Jamie Platt, BSN, RN, CLC, CPST shares her personal insights on what it’s like to be a postpartum doula. What is the role of a postpartum doula? What does it look like, and how might a doula support the breastfeeding relationship between mom and baby? A postpartum doula can take care of […]
Media – Friend or Foe?

In light of recent events, we have a special guest blog by Lindsey Zaskiewicz, LMSW. Lindsey is a licensed social worker currently employed as a clinician on a mental health and substance abuse crisis line. Prior to this role, she has several years of experience working in maternal-infant mental health, as well as direct practice with […]
[un]common sense: Managing your guilt as a Mompreneur

Today’s blog is written by Alyssa Veneklase – mother, wife, doula, and business owner. She talks about not just mom guilt, but very specifically the type of guilt we have as mothers and business owners. Enjoy! I worked full-time in an office when I found out I was pregnant, and my assistant at the time […]
Podcast Episode #17: How to Find a Babysitter You Trust

On this episode of Ask the Doulas, Alyssa and Cindy talk about how to find a babysitter that you trust to watch your kids. You can listen to this entire podcast epidode on iTunes and Soundclound. Alyssa: Hi, welcome to another episode of Ask the Doulas. I am Alyssa, and I’m here with Cindy from […]
Podcast Episode #11: Trust Your Gut

In this episode of Ask the Doulas, Alyssa talks with Cindy about the importance of trusting your gut instincts as a mom. You can also listen to this podcast on iTunes. Alyssa: Hi, welcome to Ask the Doulas. I am Alyssa, co-owner and postpartum doula at Gold Coast Doulas. Today’s show is sponsored by Cindy’s […]
Podcast Episode #10: Dealing with Modern Medicine and Your Mother-in-Law

On this episode of Ask the Doulas, Alyssa and Cindy talk about dealing with input from family members, including your mother-in-law, about parenting and about the role modern medicine plays in being a parent. You can also listen to the podcast on iTunes. Alyssa: Hi, welcome to Ask the Doulas with Gold Coast Doulas! This […]
Tandem Nursing
This article was written about four years ago by Kristin when she was tandem nursing both of her children. She recently stumbled upon it and we thought it would be a beautiful piece to share with all of you! I never imagined myself as a tandem nursing mom, it just worked out that way. My […]
Podcast Episode #9: How to Handle a Six-Week NICU Stay

On this episode of Ask the Doulas, Tricia talks about her experience with her twins staying in the NICU for six weeks. You can also listen to this podcast on iTunes. Alyssa: Hi, welcome to another episode of Ask the Doulas with Gold Coast Doulas. I am Alyssa, co-owner and postpartum doula, and today we’re […]
Sleep Training is a Four Letter Word

Sleep Training. Those two words can stir up some pretty aggressive emotions for some parents. I guess it’s because there are so many methodologies, many of which are controversial, and there are so many different thoughts on parenting and what is right and wrong. My answer is there’s no one way to do this! If […]
Make Your Hospital Room Feel Like Home

Today’s blog comes from one of our past birth doulas, Courtney Garvelink. Her experience with birth clients, as well as being a licensed massage therapist and previous HypnoBirthing instructor, makes her an expert on comfort measures in the delivery room. See what she has to say about making your hospital birth feel more like home. […]
[un]common sense: Buy them what they asked for

[un]common sense is a blog about navigating through everyday life, using some common sense tips to make it just a bit easier, and sometimes a little more fun. Alyssa is a wife, mother, and postpartum doula who has some tricks up her sleeve and wants to share them with the world. Well now, don’t you […]
Postpartum Depression & Anxiety Resource List

After our recent event at the Wealthy Street Theatre where we screened ‘When the Bough Breaks – A Documentary about Postpartum Depression’ we realized that there are many great resources available to our community, but people may not know how to find them. We at Gold Coast, with the help of Cristina Stauffer, have compiled […]
The Modern Grandparent

Understanding the Modern Parent First of all congratulations on becoming a Grandparent! Whether this is your 1st or 5th, it is a very excited time for the whole family. Gold Coast Doulas offers in-home private classes for The Modern Grandparent. We are not currently offering group classes. This 2 ½ hour class will break down […]
[un]common sense: unintentionally intentional

[un]common sense is a blog about navigating through everyday life, using some common sense tips to make it just a bit easier, and sometimes a little more fun. Alyssa is a wife, mother, and postpartum doula who has some tricks up her sleeve and wants to share them with the world. Well now, don’t you […]
Dealing with Stress

Today’s blog comes from one of our previous postpartum doulas, Alex. Her nurturing soul shines in this post, giving us her favorite tips for stress management and self-care. Take the time today, and every day, to nurture yourself. It’s no secret that stress is, inevitably, a part of life, and to some degree is healthy […]
The Big Latch On – Grand Rapids 2017

World breastfeeding week is coming up! Why do we care? Each year, World Breastfeeding Week presents many opportunities to celebrate and promote breastfeeding. From August 1-7, this global movement strives to support breastfeeding by cultivating awareness and cooperation within and between communities worldwide. One big way we come together during World Breastfeeding week […]
[un]common sense: redefining breakfast one bowl at a time

[un]common sense is a blog about navigating through everyday life, using some common sense tips to make it just a bit easier, and sometimes a little more fun. Alyssa is a wife, mother, and postpartum doula who has some tricks up her sleeve and wants to share them with the world. Well now, don’t you […]
Kerry – A HypnoBirthing Birth Story

We love hearing birth stories from our HypnoBirthing students. Kerry had a rough ride but made it through three days of labor in the hospital, smiling in the end because of the tools and techniques she learned in Ashley’s HypnoBirthing Classes. “I just wanted to shoot you a note thanking you so very much for […]
