Pacifier Weaning with Lindsay DeOliveira: Podcast Episode #275

Kristin Revere and Lindsay DeOliveira discuss pacifier weaning in the latest episode of Ask the Doulas. Lindsay is the founder of Soothe Beginnings Pacifier Company and is a Certified Baby Registry Consultant with Gold Coast Doulas. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with my friend […]
Setting Up a Feeding Support System: Podcast Episode #274

Kristin Revere talks with Lauren Scocozza, Vice President of Product for Willow Innovations, Inc., about why it is important for moms to have a feeding support system and how to set one up. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Lauren Scocozza today. Our topic […]
5 Questions Every Parent Should Ask When Hiring a Night Doula

If you’re reading this, you’re probably exhausted–or preparing to be. That’s where a night doula, or an overnight postpartum doula, comes in handy. Night doulas are trained to help support the mother and baby–or babies–right after delivery and into the first year of life. They help with overnight newborn care, sleeping, breastfeeding, physical and emotional […]
The Importance of Pelvic Floor Physical Therapy: Podcast Episode # 273

Kristin Revere and Dr. Desiree Cassell discuss how to find the best pelvic floor physical therapist for your unique needs and when to hire them on the latest episode of Ask the Doulas podcast. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Dr. Desiree Cassell. Dr. […]
Postpartum Nutrition with Maranda Bower: Podcast Episode #272

Kristin Revere and Maranda Bower talk about the importance of postpartum nutrition in the latest episode of Ask the Doulas. They also discuss postpartum planning during pregnancy. Hello, hello! This is Kristin with Ask the Doulas, and I am thrilled to chat with my friend Maranda Bower. Maranda is the CEO and founder of Postpartum […]
2024 Reflections
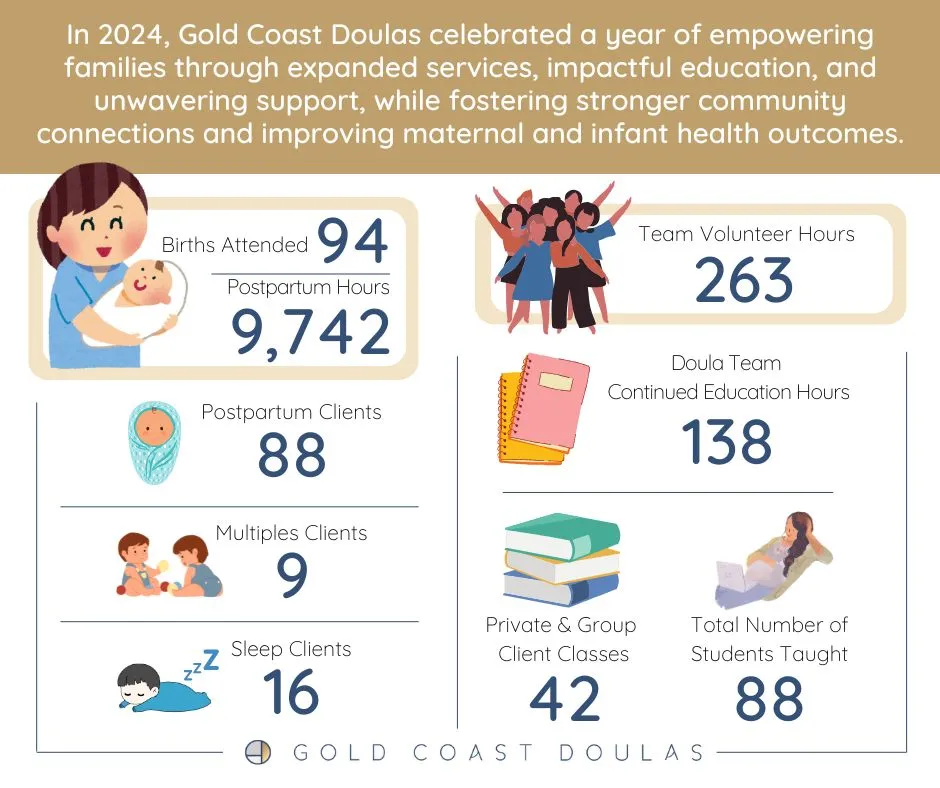
In 2024, Gold Coast Doulas celebrated a year of empowering families through expanded services, impactful education, and unwavering support, while fostering stronger community connections and improving maternal and infant health outcomes. What we did well In 2024, Gold Coast Doulas prioritized refining its operational systems and structure to fuel sustainable growth. By continuing to leverage […]


