All About Vaginal Birth After Cesarean: Podcast Episode #262
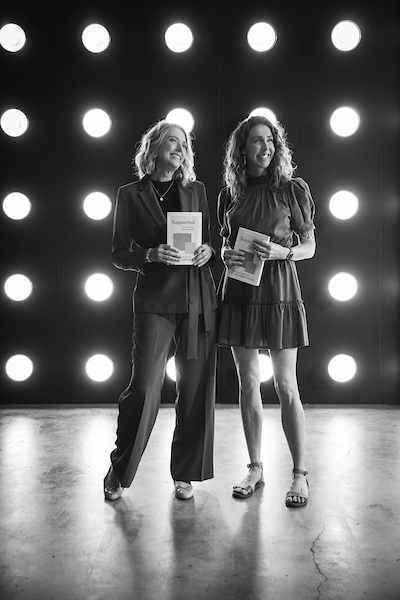
Kristin Revere and Meagan Heaton discuss VBAC preparation for families and tips for doulas supporting VBACs in this informative episode of Ask the Doulas. Meagan is the CEO of VBAC Link.
Hello, hello. This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with my new friend Meagan Heaton. Our topic today is all about VBACs. Meagan is the VBAC Link owner and founder. She’s a doula, and she’s also a VBAC mom after two Cesareans. Very impressive! Welcome to the show! I would love to hear more about your personal story, Meagan!
Thank you so, so much! It is such an honor to be here with you and be talking with your audience and sharing my story. I do love my story. I really hold it near and dear to my heart because I truly believe that my stories are what led me here today. I think that’s a lot of the times how birth doulas get into birth work, too, just based off of their own experience.
As you kind of mentioned, I did. I had two C-sections, and with my first C-section, I was young. I was very uneducated. Very, very uneducated. I actually just downloaded an app, and that’s what told me what to expect.
That’s really typical, Meagan.
I was just like, this will tell me! And it told me what size my baby was, and it told me what pregnancy symptom I might be experiencing that week. That was really about it. It just didn’t tell me much, and I was just kind of okay with that. And so when my water broke spontaneously at 39 weeks, I did what a lot of people do or are told to do or believe is what we should do because we see it on movies and on Friends and other TV shows. When your water breaks, you run right to the hospital because you’re having a baby, right?
That’s what media tells us, for sure.
It really is. And honestly, it’s even what my doctor said. Like, oh, if your water breaks, you come right in. And I didn’t know anything different. So I did. I went in, and I got there and they were like, well, you’re not really dilated. Let’s just start Pitocin. And it’s kind of weird to think back and think, oh, I was induced, because that’s now how I was seeing it then. I didn’t realize, oh, my water broke. I go in and they start Pitocin. That’s an induction. They were inducing my labor that wasn’t quite happening yet. And I was like, okay, sure. So I started Pitocin, and 12 hours later, I had made it to 3 centimeter, which to me, I was really excited about. That seemed great. Unfortunately, to my provider, it wasn’t good enough. They said no, this isn’t going to happen. Your labor is not going. Your body doesn’t know how to do it. You’re going to have to have a C-section. So I was wheeled down to a C-section. I remember laying there and hearing them talk about the weather. My baby was born November 4th, and it was the first big snowstorm of the year. One of the doctors had just gotten back from Hawaii, and they were talking about how depressing it was to be here in the snow again and not on the beach.
And this is your moment!
This is my moment! This is the time that I feel like I should be the one being talked to and about my baby and so excited, and it just was so disconnected. And my baby was born, and I of course was excited, but I also had this weird feeling of, why am I crying? Why don’t I feel more? I mean, if I’m being honest, it kind of sucked. It really sucked. It wasn’t what I had hoped for or, I guess, what I had imagined. I don’t even know why I imagined anything, because I didn’t know a lot, right? I wasn’t even educated. But it didn’t feel the way like I felt like I should be feeling.
Then I decided to learn more about my options. My doctor didn’t actually really tell me much about VBAC when I got pregnant, but I had kind of learned about it, and people kept saying, VBAC! You can VBAC! And I’m like, what in the heck is VBAC? So I would search VBACK. I just didn’t even know anything about it. I did soon find out that VBAC is vaginal birth after Cesarean. And I was like, wait, this is a thing? I can do this! So I said to my doctor, hey, do you support VBAC? And he said yeah. I was like, great. Sounds good! So the plan was to VBAC. I did start learning more about what happens in birth, and I definitely learned from my first birth that maybe the app that I got was not the only thing to go off of as far as education goes. I found myself at 38 weeks this time. My husband was out of town, and my water broke again. Oh, my goodness! I was feeling a little stressed because he’s out of town, so we got him in town, and my mom was here. He and my mom were like, you need to go. And I’m like, I don’t. I’m barely contracting. Literally, barely contracting. Maybe every 25 minutes, maybe 20. And only a 40-second long cramp.
No need to rush in, yeah.
No need to rush in, and I had learned at this point that I didn’t need to run to the doctor or to the hospital. Even though I knew that, my mom and my husband – I love them. Don’t get me wrong, I love them. But they did not know that. And I really wanted to hire a doula with this pregnancy, but we financially were not in a good space, and my husband really didn’t understand and wasn’t super on board, and I didn’t feel like fighting him hard enough. I wish I would have. But I didn’t have a doula, either. So I kind of felt pressured, and we went to the hospital. He was exhausted. He passed out. If you can imagine his rush of, oh, my gosh, my wife’s water broke. I’m in Texas! I have to get home; my wife is going to have a baby! And I think he just crashed. It was so much, and by the time he got there, he was exhausted. So he fell asleep, and I’m just sitting here, twiddling my thumbs, barely contracting. This nurse comes in and was so friendly and warm. We were chatting, and she’s like, all right, you know, not much is happening. But that’s okay, your body can do this. Let’s get you a peanut ball. Let’s get you on the birth ball. Let’s move!
Amazing! Doula-like!
So much doula-like! As we were chatting – guess what? She was a doula!
Oh, that’s why! Okay!
Yes, she was a doula, and I was like, oh, this is amazing! For me, I was like, this is a blessing. I got my doula after all! But you know what happens; at 6:00, 7:00, depending on the hospital, they leave. They’re gone. She left. And when my new nurse came in, it wasn’t the warm energy that she had brought. And it was like, well, we can’t do anything for you. We can’t give you Pitocin. We can’t do anything for you. You’re only a 1. We can’t do anything, so your doctors are going to come talk to you. So when he came in, it was very much, we’re going to go have a C-section.
It was hard. It was really hard. It was not what I wanted. My husband wasn’t super on board with VBAC, just because my doctor was saying C-section, at that point. We walked down, and I had a second C-section. It was undesired completely, but it was such a healing experience. And I think sometimes when people hear that, they’re like, wait, what? But you didn’t want that! How is that healing at all? But it really was. My husband reminded my provider, hey, she wanted to watch it in a mirror. That was something I really wanted. And I had told him that, and it was really kind of fun and special, because I was like, oh, he was listening! He was listening along the way, even though I didn’t think he was. He was. So yeah, I watched my baby be born through this mirror. It’s definitely different, but it was amazing. And the anesthesiologist was playing music, and they put my baby on my chest. It was the best thing ever. You know those belly bands that they kind of hold the monitors on with? They put that on like a tube top and stuffed my baby in that so she was secure. So for anyone listening, if you have a C-section, planned or not, that is something that really helped me. They stuck her in, and it was amazing. So amazing.
I went in the postpartum unit, and here I am, Googling how to become a doula. I became a doula quickly after that. I definitely knew in the future, I was going to VBAC. And that’s what I did; I had a VBAC! I went into labor spontaneously again. My water broke. This time I had multiple doulas. At this point, I was a doula and had so much support. I had switched providers during my pregnancy from a different provider to another provider that would truly support my VBAC and have more options. I had the most joyous experience when my midwife said, Meagan, reach down and grab your baby! I reached down, and I pulled him out. I had him on my chest. And it was really long; a 42-hour long labor. I was just so exhausted, but so high on life and birth. I just can’t explain this joy. And I remember screaming, you guys, I did it! This is possible! My pelvis isn’t too small! My body really can do this! All these things that I was told were false, were absolutely false. Soon after that is when the VBAC Link was born with a friend. We started it in 2018, and we just were like, we need to help people know more about their options for birth. Is it possible? Is VBAC really possible? Yeah, guys, it is. It’s totally possible. I just have to tell you that! It is so possible!
And I love that you explained all of your different stories, Meagan, with the Cesarean that went against all of your plans to the second surgical birth where you were able to experience more of labor, move, follow more of your birth preferences, and then have a family-centered Cesarean that gave you some healing from the first experience. And then the journey to become a doula and create this program from scratch that you needed to exist and to then be able to make even more impact by training doulas to support families and giving families more education.
Yeah, exactly! During my VBAC journey, there wasn’t a lot of information, and the information that was out there was kind of scattered all around. I still think that today. You could find how positive VBAC is and how little risk it is, to how scary it is and how you shouldn’t do it. But there wasn’t a lot of information in one place. We had ICAN. We had VBAC Facts, things like that. And it was so great, but then there was a lot of static out there. So we wanted to create a space where people could come, both parents and birth workers, and really dive deep into the nitty gritty of VBAC and what does it look like, what are some tips for people to do. Because I wanted to know what I could do to increase my chances of a VBAC. And then to have this birth worker network where people can find a doula all over the world, literally. We have doulas in Kuwait, even, who have a deeper knowledge of VBAC. I mean, I’m just here in Utah. I can’t change the VBAC world alone. Birth workers have such an amazing impact on birth and people’s overall outcomes. That’s why we wanted to broaden it past parents and reach doulas.
Yes, and I agree that back when I started as a doula, ICAN was about it. Some local support groups. But it was challenging for my clients to be able to, one, find the right provider. You mentioned switching providers later in pregnancy and finding someone who wasn’t just tolerant of VBAC birth but also more supportive and was 100% on board because providers will sometimes say, oh, yeah, I’m all for a VBAC, but really understanding and is passionate about it and who has a track record that is pro-VBAC.
Yes! I love that you mentioned that because that is honestly one of the number one tips, if not the number one tip, that I give parents who are wanting to VBAC. Find a truly supportive, truly loving provider. Someone who is up to date, that is not going to put all the restrictions on you, because even my first provider, right? Sure, yeah, we support VBAC. But in the end, he wasn’t even close to supporting VBAC. In fact, I was bullied into a repeat Cesarean. And not even just VBAC parents; I think even first time parents, really, a big goal is finding a supportive provider that aligns with you and your desires and who’s up to date with evidence based care. That’s one of the number one tips.
And then, of course, education. Education is so important. I want to say I learned the hard way, right? I want to kick myself because I should have learned! But then again, I look back and say, I didn’t learn, and that’s why I’m here today. So I go back and forth. But learn as much as you can. That is why we have the VBAC Link course, and we have a 20% off discount for any parents looking for deeper education in VBAC, and they can use BIRTH20 at checkout. But really diving into the education. Find a great provider. Hire a doula! Guys, if you can hire a doula, it’s so good. There’s actual evidence on it. I’m sure you’re aware of the evidence on doulas.
Oh, yes, but our listeners may not be. There is so much benefit, especially with VBAC families, to hiring not only a doula but also a doula who is VBAC certified through your group as well as others. I think VBAC Link has an exceptional certification program. The doulas on my team that are certified through you are highly in demand by clients. It’s not just the experience that our families are looking for, but they want the certification. It’s not just, oh, I’ve attended five VBACs. They want the education behind it and the full understanding from doulas now.
Yeah, and a lot of our doulas, I know, bring the actual book. We have an actual book, over 100 pages. They bring those to the births. If there are providers coming in saying a statistic or something like that, they can kind of fact check a little bit and have that. I just think it’s so great. And of course, I believe I was a good doula not certified in VBAC. I don’t think I was less. But I definitely have that deeper, richer knowledge and knowing like, oh, they just said that. I’ve learned that actually is not quite true. Or there’s actually an alternative to that. Let’s talk about that and really kind of help open conversation within the client and the provider, too.
Exactly, and having that community, whether it’s parent focused or the doulas, on the updated evidence based information, what the stats are, and staying current even after the certification. I think the benefit to some of the communities you created is key and just an extra bonus from going through the actual program.
Yeah, and I love that you mentioned along the way – like, evidence does change. Things are being studied, and there are certain things that, unfortunately, aren’t continued to be studied. I mean, there’s a study from 2005, and that’s the last best study we can find. But as things are evolving and updating, we’re updating that course and our doulas and parents. Even if you’ve had one birth and then four years later, you have another birth, you might want to tune in to that course. They have lifetime access to that course so they can see if there’s been updates to the course and things like that and studies that are provided in there. We always want to make sure that you are up to date on the best evidence based care so you can know and you can help guide your clients. Or if you’re a mom, you can feel prepared and educated.
I love it. So I know we’ve talked a bit about the parent perspective and some of the benefits that doulas would have in going through VBAC certification, but I would love to hear your thoughts on how a VBAC parent would be different from a parent who may be a first time family or a couple that has had multiple vaginal births.
Yeah. VBAC should not be different, right? It should just be, someone wanting to go in and have their baby just like anybody else. But it is different. The fact of the matter is that it is different. And as a doula, if I have a VBAC client, I expect and know that they may need more from me than some other first time parents or someone who’s had four vaginal births before. And it’s not just because – I’ll use myself as an example. I had never had a vaginal birth, so I was essentially just a first-time mom. There was a lot more in my past that I needed to work through, process, and understand. And I find that to be true with a lot of VBAC clients where they have experiences. And sometimes it might not even be associated or recognized as trauma, mentally. But then physically, our bodies respond as trauma, and if we don’t work through that, that can impact our future, right? It can impact the way we dilate or the way our labor starts or the way our mindset is when we walk into the birthing space, wherever that may be. I think that as doulas and birth workers, we need to expect that our VBAC clients are a little more tender, and I use tender as in just knowing that they’ve got some more. They’ve got some more to work through. I was also told that my pelvis was too small, so not only did I have experience that I needed to work through, I had a lot that I had to mentally work through to know that my body was capable. I had to re-find the belief and the faith in my body’s ability to give birth. That sucked that I had to do that. But I was so grateful for my birth doulas and for my education in VBAC to be able to do that. Not only is it different to prepare them for birth, but navigating finding support for VBAC parents – and this is nationwide – can sometimes be very difficult. And if I’m going to be super honest with you, it really ticks me off. It makes me so mad that someone has to fight so hard to find that support. It should not be that hard. It shouldn’t. But it tends to be. And that, I feel like, is a big part of what I do for my doula clients is knowing and being connected to my birthing community and all the hospitals and the birthing centers and the homebirth midwives and knowing who supports VBAC and who is that truly supportive provider, not just that tolerant, okay, sure, I’ll let you try type of provider. Yeah, I think being a birth worker, we have this space where we really can identify those people, those providers, and help guide our client to the right provider. And let me tell you – I’m going to be honest – sometimes, we’ll get a VBAC client, and they are with a provider that we know is not supportive. And we know that we might have to navigate some of the hardships that a provider may throw at someone. But if someone is asking and they want to know, hey, I’m really not feeling the support, or hey, this was said to me today; is there evidence on this? Then we’re able to do that and spend time with them. And sometimes labor can be longer with VBAC, so we have to know that, as birth workers, VBAC labors can be long. I mean, mine was 42 hours long. With my first birth, it was 12 hours long when he called it. The second one, it was 18 hours total. I was not there for very long because, again, I tried to wait it out and was waiting for my husband. But my body in particular just takes time. And a lot of VBAC moms do, just like first time moms. I mean, my body hadn’t done it before, so you have to kind of expect that sometimes labor can take a little longer.
And I’ve attended some VBAC births that are very quick, even quicker than my vaginal birthing clients. It was amazing how quick some of those ended up being, but then as you mentioned, some can be longer. As a doula, there’s no formula. Every body and baby are different.
Yeah, and I think as doulas, it’s really important, too, to kind of know a little bit more, too, on pelvic dynamics and understanding positions of babies because we know that birth workers can help so much with that, as well. So to your point, we had a VBAC mom who was kind of having a very fast labor and then it kind of stalled for an hour, and it was just a positional thing. And then within an hour later, she had her baby. So her whole VBAC was, like, six and a half hours. Wild. But yeah, I think the biggest thing for birth workers is know that VBAC clients might need some extra love and guidance and education.
So true. And as you mentioned, the mental aspect of it. It’s important for anyone who’s supporting VBAC families that there is that tenderness and that emotional support. There can be some blockages that could have happened from the past birth or births that could be carried and could stall labor. I feel like it’s so important to deal with some of that. We teach HypnoBirthing at Gold Coast Doulas, and that mental aspect of it has really been helpful for our VBAC families to do some of the fear releases and process things and really do the work in pregnancy, as you had mentioned you did with your last two pregnancies where you did so much to prepare and really wanted to ensure that birth didn’t happen to you, that you were an active participant and had the education and you could advocate for yourself, even before you became a doula.
Yes, exactly! If there’s anything I wish for anyone during their birth experience, whatever you desire or how it goes: be an active participant, just like you said. Don’t let birth just happen to you, and I think that’s really hard sometimes because we don’t feel like we have a voice, or we don’t know we can say something else, say no, or maybe later, or I don’t know these things. I think that’s really helpful where doulas come in so helpfully with that because we can kind of help you find your voice and kind of help you know your options and again facilitate that conversation versus just being told what you’re going to do or what someone is going to do to you.
Exactly. Any final tips for our listeners, Meagan?
Oh, man, yeah. I just think, get your birth team. Get your education. And birth team goes even into chiropractic care and yourself. Remember that you are an active participant on your own birth team. Sometimes I feel like clients can hire a doula thinking that the doulas are going to do it all, but if you don’t have the education yourself, that’s not good either. We want to have a whole team full of education. So educate yourself and make sure that you are prepared. Find that provider. Check into chiropractic care. Whatever it may be. Hire that doula. And really just create your space to be positive and know that it’s okay if something negative is coming in, that it’s okay to just say no, thank you, I’m going to excuse that. My mom was not a very positive person in my labor, and that was really hard for me because I wanted her to be there, but I had to be like, Mom, not now. I had to kind of exit her from my space that was safe. And I think that’s important to know, that it’s okay to do that. You are worth so much. You deserve so much. And you can have a better birth experience, and that’s our goal at the VBAC link is to have a better birth experience no matter what that may be or what you may choose. But definitely get the education.
I love it! Thank you! So as you mentioned, the VBAC Link – there are lots of different sites within the website, but what is your domain name, and how can we connect with you on social media and all of the different Facebook communities you have?
Yes! Okay, so you can find us at www.thevbaclink.com. And on there, you can find our blog. We post blogs all the time. We have so many blogs full of incredible information, studies, suggestions, all of those things. Of course, we have our podcast. You can find our podcast anywhere that you listen to podcasts. It’s The VBAC Link, and we share weekly stories of people all over the world sharing their experience and their journeys. We also have providers and doulas coming on and sharing tips and things like that. We have our resource page. We have our doula directory, so if you’re looking for a doula who is VBAC certified, go over there. It’s www.thevbaclink.com/findadoula. Type in your ZIP code; you never know, there may be a doula in your area who you can interview. Then we have our course for VBAC, for parents and birth workers. Again, we have a 20% off discount code for any of your audience members, both birth workers and parents, and you can check it out using the code BIRTH20 for 20% off the course.
On social media, just The VBAC Link. You can find us anywhere. YouTube, Instagram, Pinterest even. TikTok. Facebook. All those places. And then kind of what you said, we have some amazing groups on Facebook, so if you’re looking for a community of people with the same desires and questions and goals as you, we have a private Facebook group, and you can search The VBAC Link Community. There are some questions that you do have to answer to get in, but once you answer those questions, we can let you in, and oh, my gosh, that community is so amazing. It’s so special. Going and reading and just seeing the outpouring of love and support from the community is amazing. And then we actually have a CBAC community as well. CBAC is a new term we’re throwing out at you. That’s Cesarean birth after Cesarean. Sometimes the goal of a VBAC doesn’t always happen and it ends in a Cesarean, or someone may choose to have a scheduled Cesarean, right? And we just want you to know that we love our CBAC mamas just as much as we love our VBAC mamas. We love all of you, and we do have that group and you can search that on Facebook. It’s The CBAC Link Community.
Beautiful! Thank you for sharing all of your wisdom on VBACs and your passion, Meagan. It was a delight to chat with you today!
IMPORTANT LINKS
Birth and postpartum support from Gold Coast Doulas
All About Vaginal Birth After Cesarean: Podcast Episode #262 Read More »